Delayed reconstruction
Reshaping of the breast should be tailored to each individual patient’s desired outcome. The choice of reconstruction method depends largely on individual preferences and the cancer treatment plan. It may take several procedures to achieve the final desired aesthetic results. With delayed reconstruction, the surgeon will rebuild a natural breast shape after the chest has healed from the mastectomy or lumpectomy and after completing adjuvant therapy. A nipple can also be recreated.
Delayed reconstruction takes place weeks, months or even years after your chest has healed and the timing often depends on whether you are undergoing chemotherapy and/or radiation therapy, among other factors. Delayed reconstruction can use implants , or your own tissue (autologous reconstruction).
Advantages of delayed reconstruction: Cancer is fully treated before dealing with reconstruction and may require fewer reconstruction procedures; a mastectomy alone (no immediate recon) has a lower complication rate when compared to skin sparing mastectomy with immediate reconstruction; avoiding radiation on the reconstructed breast.
Disadvantages of delayed reconstruction: Mourning the loss of a breast can create an emotional a psychological disadvantage. In delayed flap reconstruction there is less native chest wall tissue/skin to cover and mask the flap, so that the cosmetic result may be inferior due to larger scars. This can result in a greater amount of abdominal skin being exposed on the breast which may not match perfectly with chest skin colour. Flap disadvantages. Mourning the loss of a breast; surgical operation room wait time for delayed reconstruction can be extensive, up to 2 years, depending on your location; and in a flap reconstruction one may have increased complications because two surgical sites are involved; longer surgery time and a longer hospital stay are usually involved.
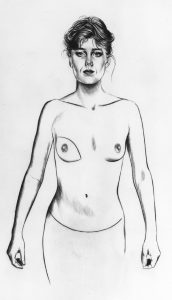
Implant based reconstruction:
In a delayed implant based reconstruction, a plastic surgeon uses a tissue expander, which is gradually filled with saline over several weeks to stretch the skin and create a pocket of skin to the desired size for the permanent implant. In a second operation the expander is removed and the permanent implant is placed. Implants may be either saline, or silicone gel implants.
Implant Based Reconstruction Advantages: Less surgical time with fewer surgical sites leading to faster recovery time; usually can be done as day surgery; fewer scars; satisfactory shape in clothing; patient has a say in final implant volume as they can choose to downsize or upsize.
Implant Based Reconstruction Disadvantages: Many appointments for the expansion process; two steps for procedure (i.e., tissue expander and implant); potential problems with implant including infection may require more surgery (less than 5% and most will respond to antibiotics); often difficult to achieve appearance of a natural breast; visual or physical distortions such as capsular contracture, rippling or bursting; pain is also possible in patients undergoing reconstruction with implants; one may need to replace implants periodically, although most implants will last a lifetime.
Implant Based Reconstruction best fits a patient who: has no history of previous radiation to the breast or chest wall or will not need radiation; does not have enough fatty tissue in stomach area for flap options; does not desire a tissue flap operation; has minimal compromised tissue at the mastectomy site; prefers shorter surgical time and recovery times, wants a more perky (augmented) looking reconstruction.
Autologous tissue reconstruction:
A plastic surgeon will use tissue from a donor site on your body like your abdomen, buttock or thigh, and move this flap to the chest to reshape into a breast. The donor tissue flap may be kept connected (or peddled) to its place of origin to preserve the blood flow (latissimus dorsi or TRAM flap). Another method is to cut the flap free and position it at the proper site of the breast (DIEP, SIEA and free TRAM flap). Here blood flow is reestablished by microsurgery. With all delayed reconstruction, flaps of autologous tissue may be the preferred option if your surgeon is not able to stretch the skin enough to make room for an implant. Flap reconstruction is often recommended in the radiation setting as this procedure bypasses some of the tissue damage caused by radiation and replaces damaged skin with healthy skin.
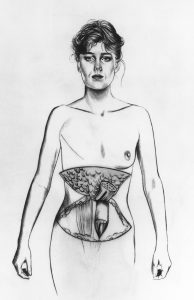
Latissimus doors flap + implant: In a lat flap procedure a muscle from the back (latissimus doors), with connected skin, fat, and blood vessels, are passed through a tunnel under the skin to the chest to replace compromised chest wall skin after radiation, or shape the pocket for a breast implant allowing for expansion of healthy vascularized tissue. The transferred tissue remains attached to its original blood supply making the lat flap procedure less complicated than other flap procedures.
In the delayed reconstruction setting the lat flap is only used with an expander due to the limitations of available skin. This makes the lat flap plus implant a 2 stage procedure, replacing the expander for an implant at a later surgery, after the skin has been stretched.
Advantages of lat flap: Muscle can act like acellular dermal matrix to protect the implant in immediate reconstruction; vessels remain connected so no reattachment is required, lessening the potential for vessel failure; no microsurgery required; less risk of flap failure; shorter procedure and hospital stay compared to other flaps.
Disadvantages of lat flap: Scarring on the back; loss of muscle function — not significant but some patients notice when performing extreme activity such as rock climbing. 2 stage procedure surgery time of 2-4 hours.
This type of reconstruction best fits a patient who has insufficient tissue for other flaps, but has compromised tissue on the chest wall which prevents use of a tissue expander alone. Lat flaps also avoid abdominal surgery.
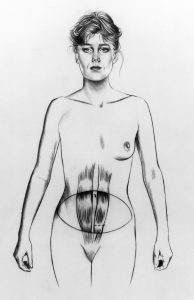
Abdominal Flap: The most common flap reconstruction surgeries will use tissue from the lower abdomen, such as the TRAM flap, DIEP and SIEA.
The TRAM implies removal of muscle which often requires a mesh to reinforce the abdominal wall; may require microsurgery.
In a DIEP flap muscle preserved but injured; less abdominal wall weakness compared to the TRAM; not all surgeons offer this procedure, depending on training and experience; requires microsurgery.
The SIEA flap may have complicated vascular anatomy, not all surgeons offer this procedure; requires microsurgery.
Advantages of abdominal flap: From patient’s own tissue; more natural look; tummy tuck; reconstruction is completed in one procedure; less muscle damage in DIEP and SIEA (as no muscle is removed) compared to TRAM. In SIEA all abdominal muscles are undamaged because no muscle is moved or even manipulated (however, this flap success varies depending on surgeon performing the procedure).
Disadvantages of abdominal flap: Long surgery, ranging from 4 to 12 hours (bilateral i.e. two sides); complex surgery requiring microsurgery for connecting blood vessels; likely removal of a section of rib (to expose blood vessels needed to connect blood supply to flap); long hospital stay 4 to 5 days; drains are required and pain management; flap must be monitored for 3-4 days in hospital to ensure blood supply is adequate; more incisions bring a greater risk of complications such as wound infection; prolonged healing.
This reconstruction best fits a patient who is concerned about using implants, has had radiation or desires fewer surgical procedures.
Other flap reconstruction surgeries:
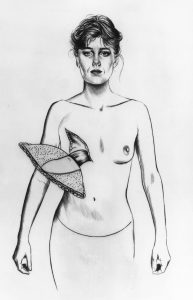
SGAP (Superior Gluteal Artery Perforator) uses tissue from the upper buttock area.
IGAP (Inferior Gluteal Artery Perforator) uses tissue from the lower buttock area.
TUG (Transverse Upper Gracilis) uses tissue from inside of thigh.
PAP(Profunda Artery Perforator) uses tissue from the inside and back of the thigh just below the buttocks.
Advantages of SGAP/IGAP/TUG/PAP: No chance of abdominal wall weakness or scarring; good tissue quality; scars may be concealed in the buttock or groin creases and may be less visible (does not apply to SGAP scars which will be visible).
Disadvantages of SGAP/IGAP/TUG/PAP: Longer more complex procedure; less frequently performed as many surgeons may not offer this; asymmetry at the donor site due to removal of tissue from one side and not other; TUG scar in buttock crease may be irritating to some; in a bilateral procedure the labia may be repositioned through stretching to close incision; less tissue available in a TUG which will limit size of reconstructed breast.
These reconstructions best fit a patient who is not a candidate for expander reconstruction of any form, does not want implants, has insufficient abdominal tissue or is not a candidate to use abdominal tissue, and wants to avoid an abdominal scar.
Learn more about the difference between TRAM and DIEP flap surgeries through an analysis of the 100 most commonly cited articles on the two procedures.
Learn more about latissimus dorsi flap surgery.
Learn about breast reconstruction using implants, skin expanders, dermal matrices and fat grafting.
Learn about possible risk factors of silicone implants.
What is Breast Reconstruction | Overview
Learn more about the different options for breast reconstruction (both immediate and delayed).